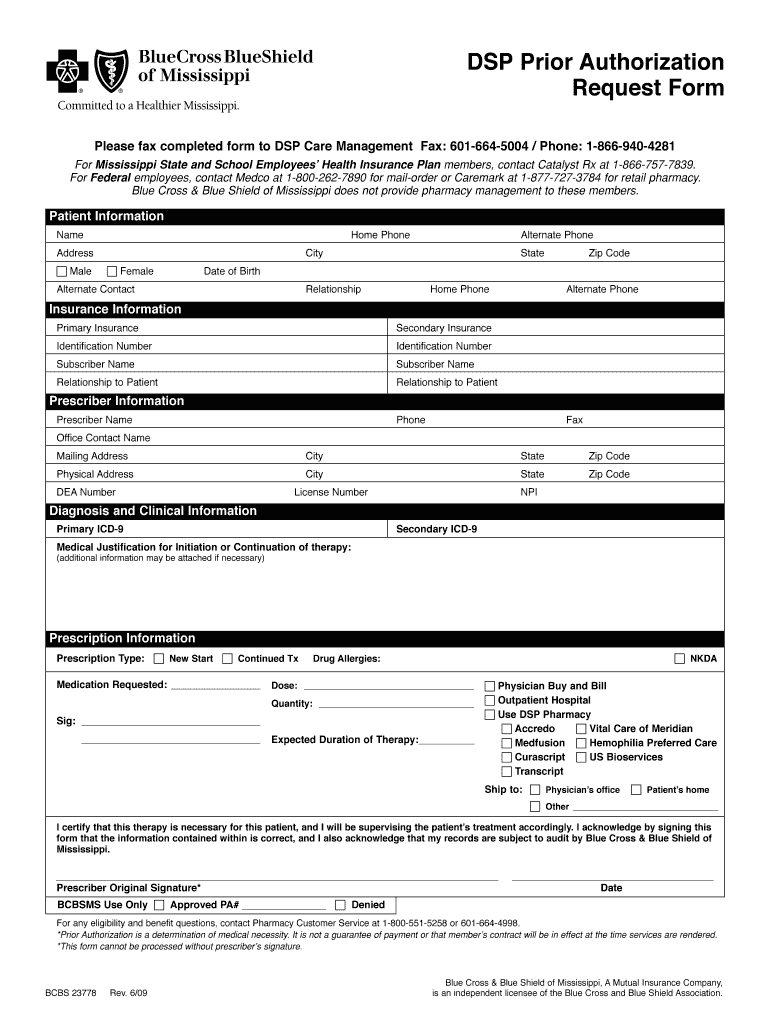
Blue Cross Blue Shield Of Mississippi Prior Authorization Form
Blue Cross Blue Shield Of Mississippi Prior Authorization Form - Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website.
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the.
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization.
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure.
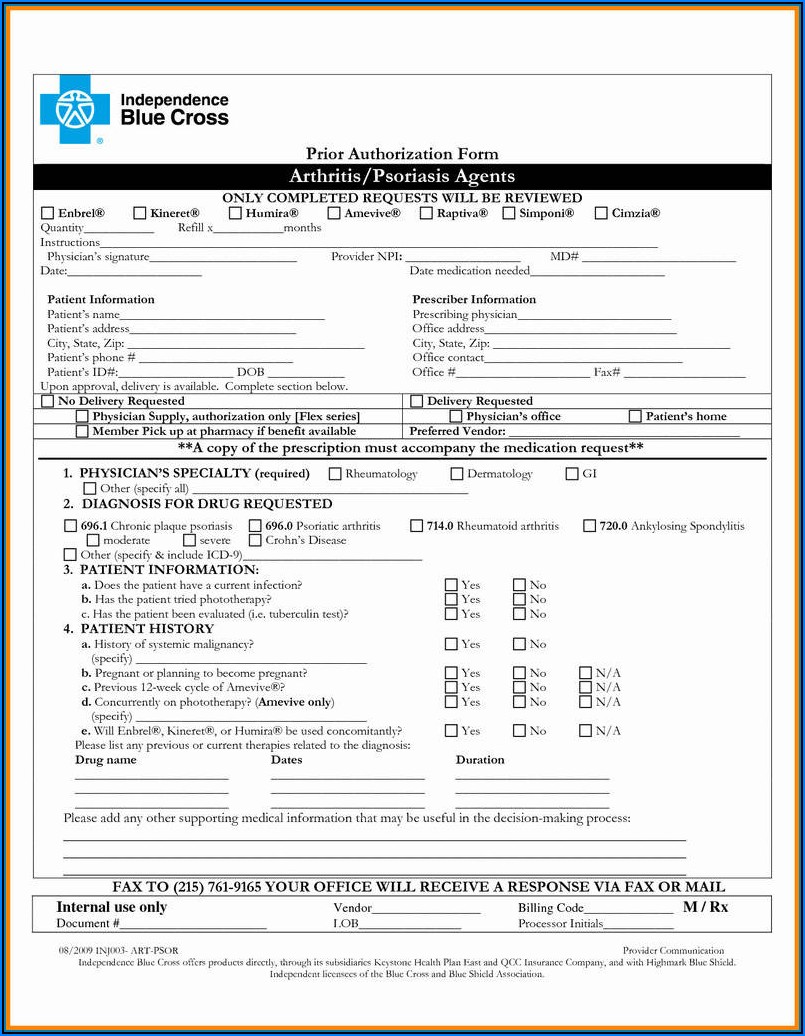
Blue Cross Massachusetts Prior Authorization Forms Form Resume
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a network provider, use the myblue provider website to request a prior authorization. If.
Medicare Plus Blue Ppo Prior Authorization Form Form Resume
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id.
Fillable Online Blue cross blue shield medication prior authorization
If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription.
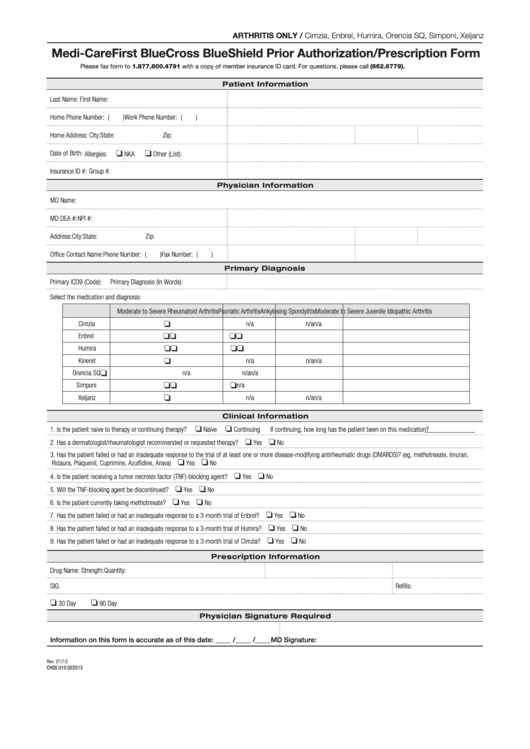
Fillable Medicare First Blue Cross Blue Shield Prior Authorization
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id.
Agreement reached between UMMC and Blue Cross Blue Shield of Mississippi
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription.
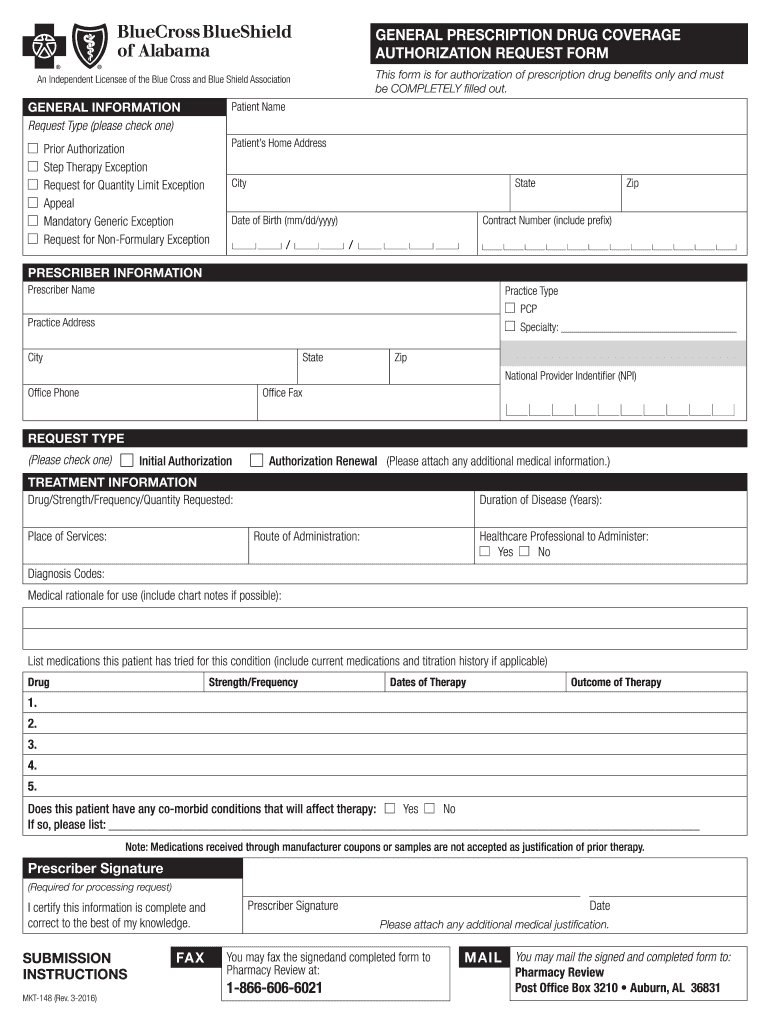
Blue Cross Blue Shield of Alabama Prior Authorization 20082024 Form
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id.
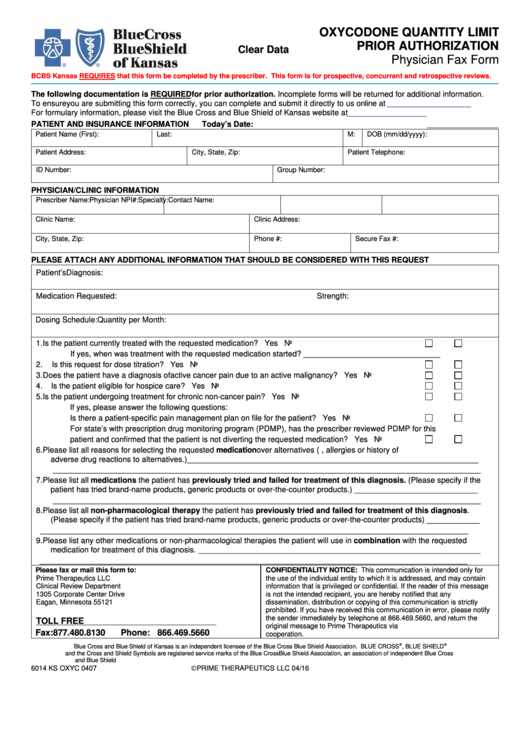
Blue Shield Highmark Bcbs Prior Auth Form
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription.
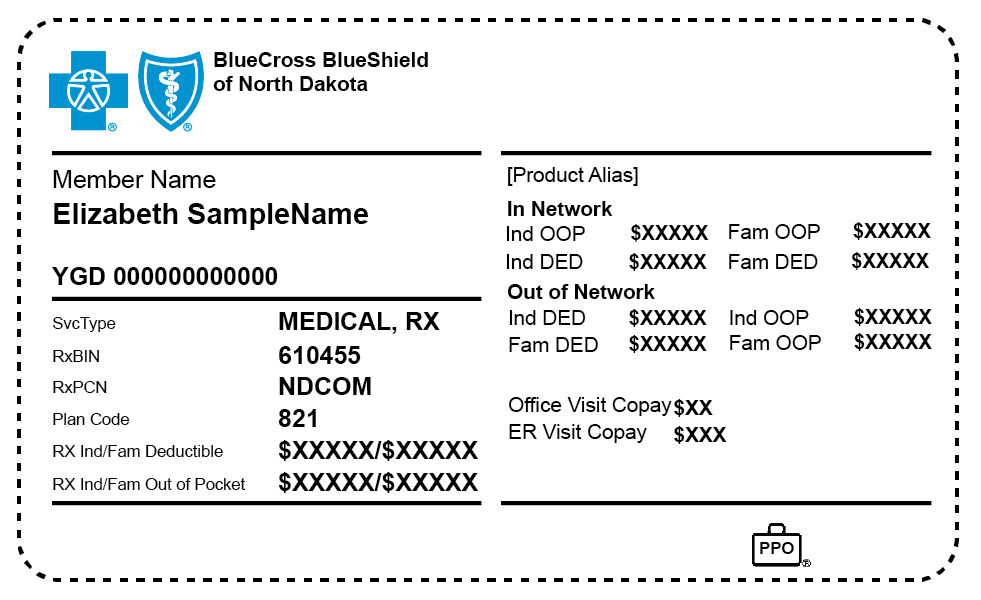
Authorized to Release Information BCBSND
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id.
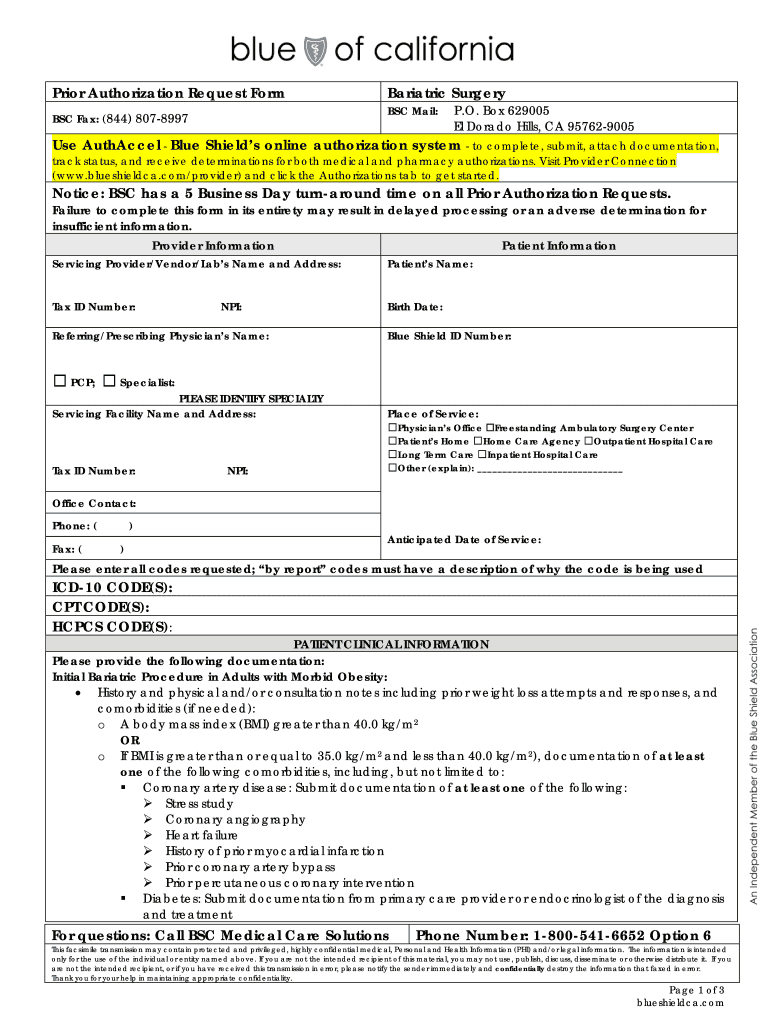
CA Blue Shield Prior Authorization Request Form Bariatric Surgery 2016
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Certain drugs must be.
Prescription Drugs Requiring A Prior Authorization Are Member/Benefit Plan Specific And Requires The Member/Patient’s Name And Id To Start The.
If you are a network provider, use the myblue provider website to request a prior authorization. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website.